Can you get an epidural if you have scoliosis?
/After having poor results with my first labor and delivery epidural, I wondered if my scoliosis was to blame—and whether I could effectively get one the second time around. Here is what I found out—and what I did.
What is an epidural?
Bruce Blaus. Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
An epidural is a regional anesthesia administered to laboring women by an anesthesiologist to reduce pain from the pelvis/lower back, down. A catheter is inserted into the epidural space near your spine through which the medication to provide relief flows.
As the catheter is fed into a space (4–6 mm on average) along your spine, scoliosis (which involves a sagittal, or sideways, and rotational curve of the spine) can affect the success of such a treatment.
My first epidural
Two things seemed to go wrong—or sub-optimally—in my first epidural. I naturally have a lower blood pressure, and epidurals further lower blood pressure, which caused me to lose consciousness. This, however, didn’t directly relate to the location of the catheter or my scoliosis. The other issue was that my left hip was still in pain after the procedure. This hot spot was likely to have resulted from slight angle variations from the placement of the catheter, which could have been affected by my scoliosis.
What the anesthesiologists said
In preparation of my second child’s arrival, I spoke to two anesthesiologists about whether I should get an epidural this time around.
Though my preference was to have a natural birth, I wanted to be prepared in case I was in a position of needing or wanting an epidural.
We discussed my low blood pressure, and they gave me good insight into how epidurals work and how people with scoliosis can receive them.
In short, the answer I received is that women with scoliosis can receive epidurals. Hooray! They discussed several factors they consider, though, in determining whether they can give someone an epidural and how effective it could be.
1. Severity
The severity of the curve can make it difficult for the anesthesiologist to find the epidural space. In addition to the sideways spinal curve there is also a rotational component in scoliosis, both of which have to be navigated in placing the catheter in the right spot. It is possible to look for the space with an ultrasound.
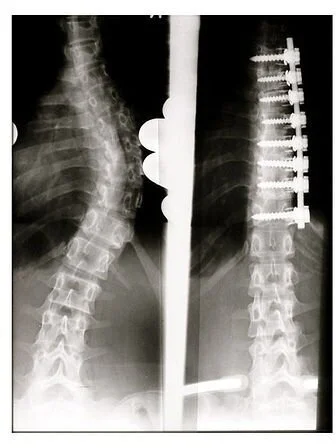
2. Fusion
Spinal Fusion (Weiss HR, Goodall D. Scoliosis. 2008 Aug 5;3:9. PMID: 18681956. doi:10.1186/1748-7161-3-9)
If the spine has been fused it may not be possible to reach the epidural space. The location of the fusions and what materials were used in the procedure will affect whether you can receive an epidural.
3. Body mass
The biggest marker for being able to receive an epidural is the spine. So, your body shape and size can impact whether you can get one. The anesthesiologist will use your spine to help determine placement, but if it is hard to find your spine, it will be hard to place the catheter in the right place.
The doctor will take these factors into consideration in determining whether you can get an epidural, and the use of ultrasound imaging can help make it possible.
My second epidural
After my first poor experience years ago, I was definitely hesitant this time around. But after discussing my situation, both doctors thought it could be done. My scoliosis is mild, I haven’t had a fusion, and I have a healthy body weight—all of which led them to believe they could assess my spine and be able to place the catheter.
Once admitted to the hospital my OB said that my baby was in an occiput posterior (OP) position, which means that the back of my baby’s head (occipital bone) was at the back (posterior) of my pelvis. While this is common, it isn’t optimal—it can make it harder for the baby to get through the pelvis, lead to start-and-stop labor patterns, and increase “back labor,” where there is more pain in the back than in the abdomen. Scoliosis is cited as a possible cause of back labor as well.
Very soon after being admitted my back pain was intense; I would tremble with agony for minutes with each contraction. Through some positioning work with the nurse, it got a little better and the pain moved more into the hips, instead of the back. But given this severe back pain, I requested the epidural.
The anesthesiologist was very clear about the process and he even felt for the rotation in my back and hips. He placed the catheter, and unlike the first time I didn’t have any residual pain or hot spots. He found the appropriate spot and I felt pretty immediate pain relief.
As a result of the epidural my blood pressure did get low, but it was monitored. I also got pretty itchy, and my contractions slowed. These are all common side effects, and in my opinion worth the back pain relief.
Different women will have different needs and circumstances, but in my case the scoliosis factors that an anesthesiologist considers did not prevent me from getting an epidural and the back labor was too intense for me to forego it. If you are pregnant and considering whether an epidural is right for you consider these factors and talk to your doctor. Having scoliosis doesn’t necessarily prevent you from receiving pain relief.
Now it’s time for the best savasana…
Get my how to set up savasana for pregnancy and scoliosis guide
Other posts in the Yoga for Scoliosis, Pregnancy, and Postpartum Series:
First Trimester Prenatal Yoga for Scoliosis
Yoga Poses for Scoliosis and Pregnancy
Review: Yoga for Pregnancy: Safe and Gentle Stretches by Sandra Jordan
Prenatal Yoga Tips
Top 5 Prenatal Yoga Poses
Torticollis and Scoliosis
Torticollis, Scoliosis, and Sensory Disorders
Review: 5 Days to Mindful Mothering by Susie Fishleder